The waiting of a baby is a time full of illusions and joys, feeling his movements inside our belly or perhaps seeing him in the first ultrasound fills us with happiness, but on some occasions, this period can be full of uncertainty and concern when they diagnose usgestational diabetes.
What is gestational diabetes?
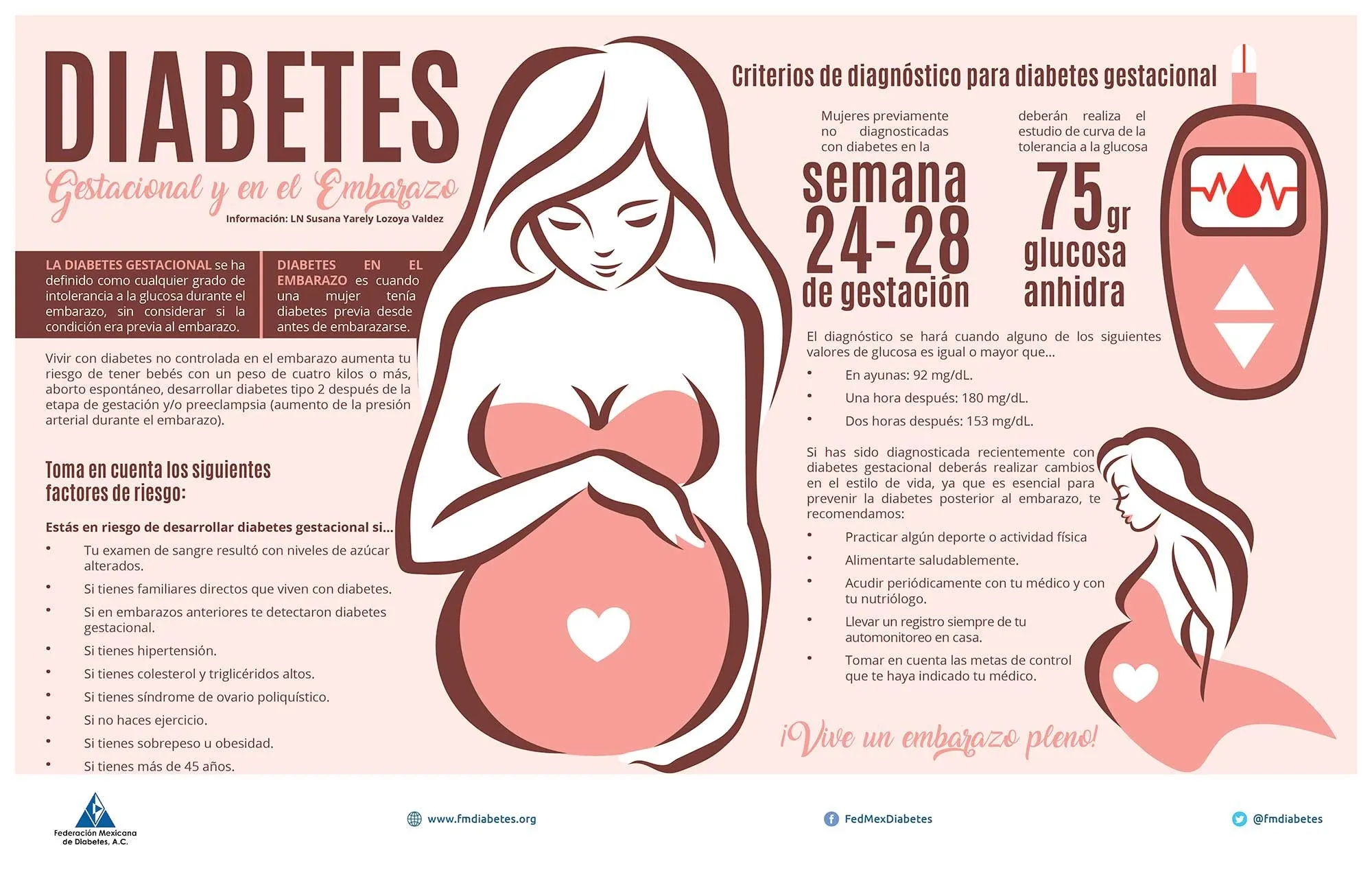
Gestational diabetes is a type of diabetes that only occurs during pregnancy, is usually detected between weeks 24 to 28 gestation and usually disappears after the baby's birth.
The chances of developing gestational diabetes increase, if:
• You have a diabetes history in your family.
• You have had an extremely big baby in a previous pregnancy.
• You have overweight.
• You have had gestational diabetes in a previous pregnancy.
• You have too much amniotic fluid.
• You are older than 25 years.
Usually pregnant women are subjected to tests for the diagnosis of gestational diabetes, during the 24 to 28 weeks.Those women with a family history of diabetes or who have had gestational diabetes in a previous pregnancy, can be subjected to testing, during week 16 to 20. The fact that you have not had the condition during your first pregnancy does not mean that noYou will develop it in future pregnancies.
What is the cause?
During pregnancy, the placenta produces hormones that act against the action of insulin causing blood sugar levels to rise beyond normal.
Generally in most women, the pancreas is able to produce additional insulin to overcome insulin resistance and maintain normal glucose levels, but sometimes, the pancreas cannot produce the additional amount of insulin necessary soThe body organs cannot use sugar to form energy and it accumulates in the blood causing what is known as gestational diabetes.
What can happen to my baby?
Gestational diabetes can be handled and controlled to prevent complications for both the mother and the baby.The key is to keep blood sugar at normal levels as soon as the disease is detected.
complications of the baby
The following two conditions can affect the baby when blood sugar is not controlled:
- Very large baby (macrosomia)
The baby receives nutrients directly from maternal blood through the placenta.If mom's blood has more sugar than normal, the baby will respond producing her own insulin.This can cause it to grow faster and larger.But even if it grows faster, do not mature at the same speed.
- Low sugar (hypoglycemia)
The baby gets used to secreting high insulin amounts to compensate for the high amount of maternal blood sugar.At birth the baby will continue to secrete large amounts of insulin but since there are no high levels of blood sugar, it can have a sudden sugar leave.
Can my baby be born with diabetes?
Having gestational diabetes does not cause the baby to be born with diabetes.The risks of the baby developing this disease are related to its family history, its weight and the lifestyle it chooses.
How should I take care of my baby and myself?
If you already diagnosed gestational diabetes, you can help control your blood sugar following these points:
Check your blood sugar daily,
Follow a special feeding plan.Remember that the amount of weight you should increase during pregnancy will be determined by the weight you had before getting pregnant.The total amount is not as important as the increase isWeekly weight.
Exercise (ask your doctor before starting it)
In case the sugar level does not reach normal figures following the previous steps, the doctor will prescribe insulin.Remember that it is not advisable to use oral medications for diabetes control during pregnancy, as they can affect the baby.
Can my baby insulin affect insulin?
The insulin that injected you will not affect the baby.Remember that insulin has the effect of lowering your blood sugar to avoid the complications mentioned in Table 1. The dose and the frequency of insulin will determine your doctor.
Where can I inject insulin?
Thinking about putting an insulin injection may worry.After putting your first injection, it will surprise you how comfortable it can be.The needles for today's insulin injection are very thin and short.
During pregnancy, the same injection sites can be used that are normally used, that is: thighs, arms, abdomen and buttocks.However, at the end of pregnancy, the skin of the stomach can be very stretched and with little fat under the skin, so you can choose an area on the stomach side where there is more fat.
Although it is unlikely that an insulin needle penetrates very deeply and arrives at the baby, it is recommended to use short needles to feel safer.Remember to ask your doctor.
Is my childbirth different for diabetes?
Childbirth must be equal to any pregnant woman who does not develop complications.Gestational diabetes should not prevent you from having a normal birth.As long as the baby is growing normally and is not very large.A very large baby will require a caesarean section.
What will happen to my baby after birth?
Immediately at birth the baby will review its blood sugar level.If blood sugar is low, it will be given glucose.Usually, as a precaution, mothers babies with gestational diabetes are placed in a special care area to observe their blood sugar levels, during the early hours after their birth.
What will happen to my diabetes after my baby's birth?
As soon as the baby is born and the placenta is removed, blood sugar must return to normal.However, this does not happen to a small percentage of women.You must make another blood glucose test six weeks after the baby is born, to make sure your blood sugar is normal.
It is important to remember that women who develop diabetes during pregnancy are very likely to develop diabetes throughout their lives.
Bibliography
1 American Diabetes Association Clinical Education Series, Medical Management of
Pregnancy Complicated by Diabetes, Third Edition, pp.114-115, 2000
2. Philopopson EH, Super DM: Gesting Diabetes Mellitus: Does It Recur in Subsequent Pregnancy?Am J obs gynecol 160: 1324-31, 1989
3. COUSAN DR, CARPERT MW, O'SULLIVAN PS, CARR, MR: GESTATIONAL DIABETES MELLIUTS: PREDICTORS OF SUBSECENT DISORDEDED GLUCOSE METABOLISM.Amerian J Obstet Gynecol 168: 1139-45, 1993