The results were announced in an article published in ‘The Fasb Journal’.They also appear highlighted in the Research Highlights section of the magazine ‘Nature Reviews Endocrinology’
FAPESP/DICYT A study carried out at the University of Campinas (UNICAMP), in São Paulo, Brazil, showed that a substance that secretes the muscles in response to physical exercise-Interleucin 6 (IL-6)-increases the survival ofInsulin -producing pancreatic cells in a type I diabetes model.
"Apart from strengthening the importance of physical activity in the control of diabetes, this discovery opens the way to the development of drugs that simulate the action of the IL-6 in the pancreas," said Claudio Cesar Zoppi, a researcher at the laboratory of the laboratory ofEndocrine and metabolism pancreas of the Department of Structural and Functional Biology of the UNICAMP, and one of the authors of the article.
Type I diabetes is caused by the autoimmune attack on insulin producers, the researcher explained.As cells die, hormone production becomes insufficient to control blood sugar levels.
Recent studies had already shown that, in carriers of type I diabetes and also type II (cases in which insulin production is high, but there is a resistance of certain cells to hormone action), the adoption of a programPhysical training improves both survival and beta cell function.
Results that appear in scientific literature also indicate that physical activity not only turns the environment of the pancreas more favorable to the survival of cells - to reduce glycemia, inflammation and triglycerides, for example - but also induces direct adaptations inbeta cells.
"The question we try to answer within the framework of this study was the following: What molecular and intracellular mechanisms are altered in beta cells due to physical exercise, and how does that signal reach the pancreas?" Said Zoppi.
To unveil this enigma, various experiments were carried out during the Flávia Postdoctorate Maria Moura de Paula, carried out with the FAPESP scholarship and under the supervision of Professor Antonio Carlos Boschero, of the Unicamp.Boschero and Zoppi are also linked to the Center for Research in Obesity and Comorbidities (OCRC), one of the Research, Innovation and Dissemination Centers (CEPIDS) of the FAPESP.
In one of the models, he submitted for two months to healthy mice to a physical resistance training program, that is, long -lasting and low intensity.After this period, the researchers extracted samples of pancreatic islets, the structures in which beta cells, insulin producers are located.
“The next step was to simulate, in vitro, the autoimmune attack on beta cells, analogous to what happens in type I diabetes carriers. For this we incubate the islets of the mice with the pro-inflammatory cytokines interferon-gamma and interleucin1-beet, the same secreted by defense cells, ”said Zoppi.
The islets of the trained mice presented a mortality index by 50 percent lower than those of the sedentary mice, belonging to the control group.Likewise, the researchers observed that there was a lower production of nitric oxide and the fragmented Caspasa 3 protein, substances that signaling the cell that is time to enter into the process of apoptosis (programmed cell death).
“But pancreatic islets have other types of cells, including the alpha cell and the delta cell.We needed to demonstrate more specifically the effect of exercises on beta cells, ”he saidZoppi
In vitro experiments were then made with two cell lineages of beta cells: the INS-1E lineage (from rat from rat) and the MIN-6 (from mouse).The stimulus of physical exercise was simulated pharmacologically, explained the researcher.
“We incubate a muscle cell lineage with a drug known to induce the same adaptations that generate resistance exercises.Subsequently, we incubate beta cell lineages only with the culture medium of those ‘trained’ pharmacologically.In another experiment, beta cell lineages were incubated with whey of animals undergoing resistance training.In this way, it was possible to simulate the cell environment of a trained animal, ”he said.
The results were similar to the one observed in the experiment conducted with the islets.The mortality of INS-1e cells "trained" was 50 percent lower than in the control situation.
“It was still discovering which molecule would be the interlocutor in that conversation between the muscle and beta cells.We imagine that a possible applicant would be the IL-6, because muscle contractions stimulate the release of large amounts of that cytocin, ”said Zoppi.
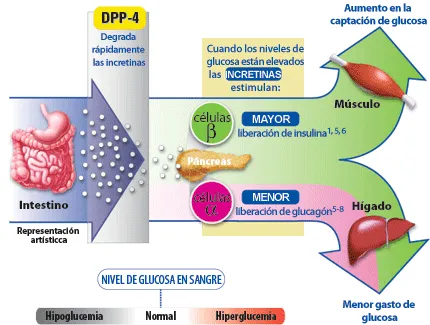
Likewise, according to the researcher, recent studies had shown that IL-6 is an important signaling between tissues, mainly those that take part in the glycemic control, sending signals from the muscles to organs such as the liver and the hypothalamus.
To verify this hypothesis, the researchers repeated the initial experiments and observed that, when a pharmacological inhibitor of the IL-6 was added to the culture medium, the protective effect of the exercise was abolished.
To reinforce the results, the group used a genetically modified mouse model so as not to express the IL-6.Animals were submitted to training and, after two months, the islets of control animals (sedentary) were treated under the same previous conditions with the serum of trained animals that did not express the IL-6.
"We repeat the same experiment and, in that case, the physical exercise had no protective effect on beta cells," said Zoppi.
The results were announced in an article published in The Faseb Journal.They also appear highlighted in the Research Highlights section of Nature Reviews Endocrinology.
new medications
Currently, De Paula performs experiments with islets of human donors in the Experimental Medicine Laboratory of the Free University of Brussels, in Belgium, to try to repeat the results observed in mice.The Unicamp group also plans to carry out a study with a view to prospecting molecules capable of activating the same signaling route of the IL-6 in the pancreas.
“I think we cannot directly use the IL-6 as a treatment, because it presents multiple actions, and, depending on the context, it can have anti or pro-inflammatory action.Maybe we can find an analogue with therapeutic effect, ”said Zoppi.
The investigation is carried out within the framework of the thematic project entitled molecular mechanisms involved in the dysfunction and death of pancreatic beta cells in diabetes mellitus: Strategies for the inhibition of these processes and for the recovery of the island mass in different cellular models and animals, coordinated by Boschero.