A treatment that is directed to rebel immune cells in people with type 1 or type 2 diabetes could help them even years later, find a new study.
For treatment, researchers take blood from a person with diabetes and separate the cells from the immune system (lymphocytes).They briefly expose those cells to stem cells of the umbilical cord of a baby who is not related.Then they return the lymphocytes to the patient's body.
Researchers have called this treatment "stem cell education therapy", because by exposing themselves to stem cells, wandering lymphocytes seem to learn again the way they should behave.
"The stem cell education therapy is a safe method" with a long -term effectiveness, said the leading author of the study, Dr. Yong Zhao, an associated scientist at the Medical Center of the University of Hackensack, in New Jersey.
Type 1 diabetes is an autoimmune disease that occurs when the body's immune system attacks the beta cells of the pancreas, which produce insulin.This leaves people with type 1 diabetes with little or no insulin.They need insulin injections to survive.
The researchers have long since thought that any cure for type 1 diabetes would have to stop the autoimmune attack, at the same time that beta cells are regenerated or transplanted.
But Zhao and his team developed a new method for the problem: educating immune cells that have been destroying beta cells so that they stop attacking.
In type 2 diabetes, Zhao said that the dysfunction of immune cells is responsible for chronic inflammation that causes insulin resistance.When someone is insulin resistant, their body cells cannot use insulin properly to bring food sugar to cells in order to use it as energy.Instead, sugar accumulates in the blood.
The researchers expected the education of stem cells to help reduce insulin resistance in people with type 2 diabetes.
In previous trials, the treatment was significantly promising with the data collected in up to one year.The researchers also showed that the treatment was safe.
The current study observed the data collected for four years on 9 patients with type 1 diabetes in China.
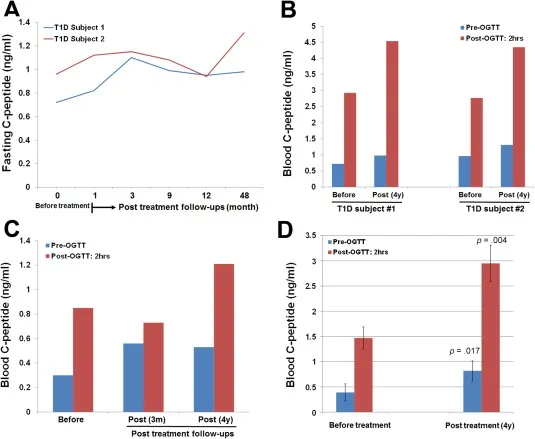
To see how well the treatment works, the researchers measured the C peptide, a fragment of protein that is a secondary product of insulin production.
Two people with type 1 diabetes who received a stem cell education
Another patient of type 1 diabetes had had the disease for four years when he received the treatment.In any case, it had improvement in C peptide levels, but it was not considered in remission.The other six people with type 1 diabetes experienced reductions in C peptide levels over time.The study authors said this suggests that more than one treatment is needed.
"As it was a first essay, patients only received a treatment. We now know that it is very safe, so patients can receive two or three treatments," Zhao said.
The researchers also observed six patients with long -term severe diabetes (from 15 to 24 years).They found that a treatment helped four patients achieve normal C peptide levels and keep them during four years.
"In four of patients with type diabetes2, the C peptide is very stable after treatment, "said Zhao.
In addition to helping people with diabetes, Zhao said treatment could also help in other autoimmune diseases.These could include alopecia areata (which causes a significant and sudden loss of hair), lupus, hashimoto's thyroiditis, and Sjogren's syndrome, he said.
Julia Greenstein, vice president of research on discoveries of the JDRF (which was previously known as Juvenile Diabetes Research Foundation), said that Zhao and her team have shown that "platelets seem to have a direct effect on beta cells," helping somehow somehowTo beta cells.
"This research is interesting, but you have to reproduce it," he said
Both Zhao and Greenstein noted that diabetes seems to be slightly different in Chinese populations, with respect to Westerners.So it is not clear if this treatment would be equally beneficial in people of European descent.
To find out, Zhao plans to perform a clinical trial on the new treatment in people with type 1 diabetes at the Hackensack Medical Center.
The study appears in a recent edition of Stem Cells Translational Medicine.
Sources: Yong Zhao, M.D., Ph.D., Associate Scientist, Hackensack University Medical Center, Hackensack, N.J.;Julia Greenstein, Ph.D., Vice President, Discovery Research, JDRF;July 7, 2017, Stem Cells Translational Medicine