The skeletal muscle is the tissue responsible for eliminating blood glucose after meals, so the damage to this tissue accelerates the progression of diabetes.
Type 1 diabetes is a chronic disease encompassed in the so -called 'autoimmune pathologies', in which the immune system mistakenly attacks the organism itself - in this specific case, to the beta cells of pancreatic islets, responsible for insulin production-.
Consequently, and since this insulin is the hormone responsible for the cells to capture the glucose of the blood to produce energy, the bloodstream ends up carrying an excess of glucose, which can end up causing damage to multiple organs of the body.
This is the case, among others, of the eyes - diabetic retinopathy - and the kidneys - diabetic negatter.And also, of the muscles.And it is that as a study led by researchers from McMaster University in Hamilton (Canada), type 1 diabetes causes progressive damage in the muscle tissue that can increase, and much, the risk of disability.
As Thomas Hawke, director of this research published in the "Diabetology" magazine explains, "now we already know that even people with physically active diabetes experience changes in their muscles that can damage their ability to handle blood sugar.And since this complication can contribute in the long term to a faster disability development, we must try to address it much earlier ».
mitochondrial damage
In the study, the authors analyzed the samples of muscle tissue taken to young adults with and without type 1 diabetes and physically active.In fact, all participants fulfilled the recommendations on physical exercise prepared by the Canadian Diabetes Association - basically, 150 minutes of aerobic activity and three sessions of resistance exercise per week.
The results showed both structural and functional alterations in mitochondria - this is, the responsible organelles process nutrients and oxygen to generate the energy required by cells - of the muscle cells of patients with type 1 diabetes. And these 'alterations' 'alterations'Were they important?Yes, and a lot.Not surprisingly, they caused mitochondria to have a lower capacity to produce energy for muscle and, in addition, release greater amounts of reactive oxygen species - or what is the same, of ‘free radicals’, very harmful to cells.
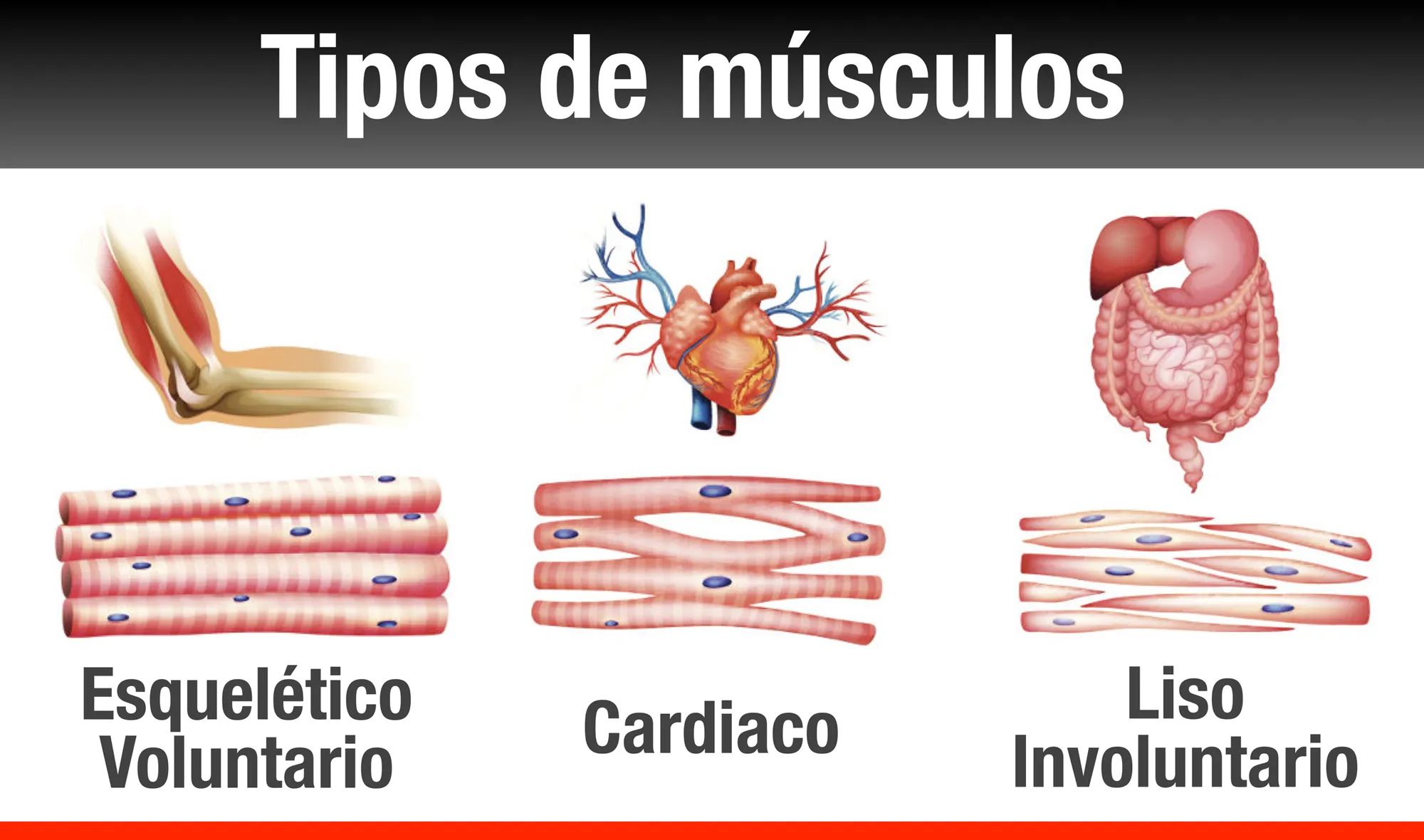
The skeletal muscle is our largest metabolic organ and the main tissue to eliminate blood sugar after meals.
As the authors indicate, "these changes can lead to a" decreased "metabolism, to a greater difficulty in controlling blood glucose and, if not being treated, at an accelerated rate of disability development.Thus, our work adds poor muscle health to the list of complications of type 1 diabetes, including neuronal damage, cardiovascular disease and kidney disorders ».
It should be taken into account that, as Christopher Perry, co-author of the research, recalls, «the skeletal muscle is our largest metabolic organ and the main fabric to eliminate blood sugar after meals, so we must maintain the muscle sohealthy as possible ».
more exercise?
In short, type 1 diabetes causes damage to muscle cell mitochondria and, therefore, in all muscle tissue.And since the muscle is absolutely essential to capture excess blood sugar, the control of glucose levels - or what is the same, of diabetes itself - looks remarkably difficult, which increases the risk thatthere is adamage to the rest of tissues and organs.
As Christopher Perry points out, “we believe that these dysfunctional mitochondria are those that are causing the muscle not to use glucose properly.A process that, in turn, damages muscle cells.We have really surprised us to observe this muscle damage in young people with type 1 diabetes that practice regularly.
But is there nothing that can be done?Well yes.It is well known that regular aerobic exercise increases the amount of mitochondria in the muscle, which helps muscle cells to consume more glucose and be more efficient.Therefore, it is possible that people with type 1 diabetes require more aerobic exercise than recommended in the guides.
As Christopher Perry concludes, "given the new evidence, it is necessary to review the clinical practice guides for type 1 diabetes and rethink the recommendations on physical exercise for this population of patients in order to safeguard their health."