Researchers at the UAM (Spain), in collaboration with the University College London (United Kingdom) and the University of Salamanca (Spain) have shown that for vascular damage to diabetic patients, in addition to the elevation of blood glucose,It is necessary that vascular cells are previously inflamed.
Cardiovascular diseases are the main cause of disease and death in patients suffering from diabetes.The elevation of blood glucose (amount of blood glucose) is a typical characteristic of this disease.For a long time, it has been proposed that the increase in blood glucose (hyperglycemia) has beenof myocardium or cerebral stroke.
Based on this hypothesis, it was thought that an effective way to reduce the mortality of diabetic patients would be to control their blood glucose very closely, so that it was as close as possible to normal values.However, this approach has not had the expected success, since various clinical studies show that the strict control of blood glucose does not reduce the cardiovascular mortality of these patients in the long term.
Now, within the existing controversy, the Farmavasm Research Group (Vascular Pharmacology and Metabolism), in the Department of Pharmacology of the Faculty of Medicine of the Autonomous University of Madrid, led by the profs.Carlos F. Sánchez Ferrer and Concepción Peiró Vallejo, in collaboration with Prof. Salvador Moncada, of the University College London, and the Profs.Juan P. Bolaños and Emilio Fernández, from the University of Salamanca, has proposed a mechanism that can explain under what conditions the high glucose produces particularly vascular damage.
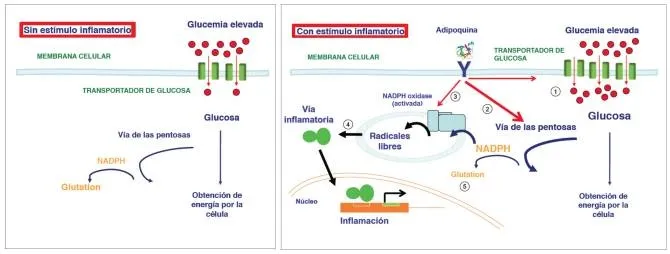
These researchers have shown that, in human vascular cells, glucose entry is not modified when their extracellular concentration increases, except when the cells are previously inflamed, a situation in which their transport increases through the cell membrane and its use byThe cellular metabolic pathways.
Effect of high blood glucose on the inflamed vascular cell.(Photo: Modified from Peiró et al, Cardiovasc Diabetol 1; 15: 82, 2016)
In these inflamed cells, in addition, a part of this excess glucose consumed is diverted by a specific metabolic route, called the Pentosas via, which increases the production of the reduced form of a compound known as nicotinamide adenine Dinucleotide phosphate (NADPH).
“This compound, which in the absence of inflammation holds a fundamental role in the formation of one of the main cell antioxidant mechanisms, glutation, has a diametrically opposite action in previously inflamed cells.In these circumstances, we have observed that the increase of NADPH is used as a substrate of a pro-oxidant enzyme, the NADPH-Oxidase, which produces free radicals and exacerbates inflammatory processes, ”explains Carlos Sánchez Ferrer, a researcher of the Department of Pharmacology of the UAM.
Therefore, the authors of the work, published in Cardiovascular Diabetology, maintain the hypothesis that the simple increase in blood glucose does not justify the vascular damage associated with diabetes since, under normal conditions, the vascular tissue has mechanisms capable of regulating theInput and use of glucose.However, hyperglycemia can exacerbate a previous or simultaneous inflammatory vascular response, a situation that is common in diabetes, in which a characteristic pro-inflammatory environment originates.This situation, which is known as chronic low -grade inflammation, also occurs in other cardiovascular diseases andIts origin is still little known.
One possibility that is increasingly strength is that it is produced by compounds called adipoquins, which are secreted by adipose tissue in situations such as obesity, which is a circumstance that is largely associated with the most frequent type of diabetes (diabetesType 2 Mellitus)."If the hypothesis is correct, the prevention of vascular pathology associated with diabetes would not only require blood glucose control, but also to develop therapeutic strategies to reduce the pro-inflammatory environment," says Carlos Sánchez Ferrer.
“In this sense, in addition to changes in lifestyle, such as physical exercise or weight loss, it is possible that new drugs designed to prevent the effects of pro-inflammatory adipacins may have in the future a relevant role to prevento Treat the development of cardiovascular diseases associated with metabolic diseases, ”concludes the researcher.(Source: UAM)